Before my dissociative symptoms intensified around 2019, I was actively engaged in life as a prolific student and researcher. But once my dissociative symptoms started flaring up in my adult life, I became dysfunctional and struggled to understand or engage in the external world. It’s taken me long time to mostly get back on my feet where I am today, but I can now definitely say that, along with therapy, naltrexone has enabled me to properly engage with and advance in life again.
Given that naltrexone is not widely known as a treatment for dissociation, I have written this post to share my experience using naltrexone to address my dissociative symptoms.
TL;DR: I take 4 mg 3x a day of naltrexone, which helps alleviate my dissociative symptoms. It is hypothesized that individuals who experience early childhood trauma may have fewer opioid receptors, which means that even minor releases of endogenous opioids could saturate these opioid receptors, leading to dissociative symptoms. Opioid antagonists can prevent individuals from responding to opioids, which could potentially relieve dissociative symptoms.
My background#
In March of 2022, I bought the book Neurobiology and Treatment of Traumatic Dissociation which introduced me to the idea of using naltrexone, an opioid antagonist, to treat dissociative symptoms. From my awareness, the information in this book isn’t discussed much elsewhere in the academic literature, making the use of naltrexone for dissociation not well known.
In November 2023, after several years of disfunction and desperation, and after trying 5 different psychiatric medications1 to help treat my dissociative symptoms, I asked my psychiatrist if I could try naltrexone. Now, after ~8 months of using naltrexone, I can confidently say that it has significantly helped to reduce my dissociative symptoms.
My dissociative symptom profile#
My main symptoms have been purely dissociation—I was so much in a daze that I had difficulty understanding where I was in life and thus was practically unable to engage in or advance in life. This very heavily impacted my brain function, as I was essentially a time-blind, disengaged, passive observer to life. I effectively experienced no emotions and spent much of my time in a spacey dissociative state. My presentation of DID is polyfragmented, and I would switch 10-100+ times a day, often with (mostly partial) amnesia. All of this rendered me unable to adequately engage in work, and for about a 3 year period, my life was stagnant. More of my symptoms are described in the posts here.
I think it’s important to note that I do not exhibit behavioral symptoms often associated with dissociative identity disorder, such as self harm, disordered eating, suicidality, or substance use issues. I believe individuals who do experience any of these may have a different experience on naltrexone than me—the dissociative symptoms that naltrexone may help reduce may be covering up some of these behaviors, thus naltrexone may make behavioral symptoms worse. Also, other than autism, I do not have any other co-morbid disorders. I am not a medical professional making this claim, this is entirely a hunch.
Endogenous opioids and dissociation#
This section summarizes my insights and understanding of Neurobiology and Treatment of Traumatic Dissociation. For more details, I highly recommend reading the source.
From mice studies, it is hypothesized that people who experienced early childhood traumas may have a reduced number of opioid receptors, specifically in the thalamus and cingulate gyrus. With a diminished number of receptors, the opioid system’s ability to regulate neural function is likely significantly impaired. Since there are fewer opioid receptors, those receptors are likely to be saturated quicker resulting in heightened parasympathetic activation, including dissociation, even in reaction to minor releases of endogenous opioids. Additionally, prolonged stress increases responsiveness to endogenous opioids, meaning those who experienced long-term stress and trauma are likely to have a stronger reaction to these opioids.
Effects of opioids#
- Endogenous opioids are released in response to stress, affecting pain perception, depressing respiration, and activating the parasympathetic nervous system (PNS), leading to a range of responses in trauma survivors
- Parasympathetic defense responses triggered by opioid release include withdrawal, helplessness, submission, and numbing, which are primitive survival mechanisms that can manifest as dissociation
- The PNS is responsible for inhibition, withdrawal, and dissociation: the remnants of the death-feigning behaviors of lower animals, which shows how the body’s response to trauma can lead to states of profound emotional and physical shutdown
- Endogenous opioids have addictive potential, which can explain their role in traumatic reenactment
- Opioids facilitate passive defense responses such as freezing and submission, inhibiting active defense responses like fight or flight, which can explain why some trauma survivors may exhibit immobilization or dissociation instead of active coping strategies. Opioids inhibit avoidance and escape from physical threat, as well as aggressive behavior that can fend off potential attackers
- Opioids play a significant role in modulating memory, particularly concerning traumatic experiences. They can interfere with memory consolidation processes, leading to amnesia and potentially fragmented or dissociated recollections of traumatic events
- The opioid system may obstruct neuroplasticity, which is crucial for learning and recovery from trauma. Excessive activation can inhibit the brain’s ability to adapt and reorganize itself in response to new experiences, hindering emotional and cognitive healing
- Opioid activation can lead to dysregulated affective responses, where extreme emotions may manifest without conscious awareness
Opioid antagonists#
Opioid antagonists inhibit the effects of both exogenous (external, like heroin and fentanyl) and endogenous (naturally produced) opioids by binding to opioid receptors without activating them. This blockage prevents the body from responding to opioids.
While there are multiple types of opioid antagonists, naltrexone is recommended for dissociative symptoms.
Naltrexone, an opioid antagonist#
Dosing#
Following the guidelines of Neurobiology and Treatment of Traumatic Dissociation, I am taking 4 mg naltrexone 3x a day (0.06 mg/kg of body weight). Oral naltrexone has a half-life of ~4 hours, so spacing doses out through the day is necessary to have the desired effects. Because the 4 mg dose I take isn’t a standard dosage for naltrexone, I have to get this dose made at a compounding pharmacy, and it is not covered by insurance. It costs me $1.25 per capsule, $3.75 a day, or ~$114 a month.
Naltrexone is typically used for opioid/alcohol use disorders and is prescribed as 50 mg tablets to be taken 1x a day. There is also usage of naltrexone at lower doses to treat a variety of ailments, often called “low-dose naltrexone” (LDN). A VERY IMPORTANT NOTE: standard LDN dosage guidelines are different than the dosing recommended for dissociation, even if the individual capsules for standard LDN and dissociation come in similar doses. For standard LDN, typically the user takes a low (1.5-6mg) dose of naltrexone 1x a day, usually at night. The theory for LDN is that at the small dose taken 1x a day temporarily blocks opioid receptors which then triggers a rebound effect where the body then boosts the production of endorphins, which act as natural pain relievers. This is different than the dosing and desired effect of using naltrexone for dissociation. For dissociation, we want to consistently block opioid receptors throughout the day, so the rebound effect that’s desired for standard LDN dosing is the opposite of what is desired to treat dissociative symptoms. While standard LDN involves taking a low dose of naltrexone 1x a day, for dissociation, one should take a low dose of naltrexone 2-3 times a day.
Side effects#
When I first started naltrexone, I was prescribed 50 mg to be taken 1x a day, which is the standard dose of naltrexone. I decided to taper on and started at 12.5 mg. On this large dose of naltrexone, I experienced pretty severe side effects, including vomiting, a severe throbbing headache, shakiness, abdominal cramping, and sweats. These side effects started about 6 hours after taking the first dose, and I was effectively unable to function and had to sleep off the side effects. From the naltrexone subreddit, it seems like many people experience these side effects for a few days to several weeks. I only took two doses before deciding to stop and reassess.
A few weeks later, I started a lower dose, aiming for 4 mg 3x a day. Over the span of a few weeks I tapered on, starting by taking 0.5 mg 3x a day, then 1 mg, then 1.5, and eventually reaching 4 mg 3x a day. I did not experience any side effects doing this. When I skip a dose, I sometimes experience a mild headache.
This past summer, in order to better understand how naltrexone was affecting me, I briefly stopped naltrexone without tapering off, and do not believe I had any side effects from abruptly stopping. When I came back on naltrexone, I immediately started back at 4 mg 3x a day and experienced a mild headache and became nauseous easily. These side effects went away in ~2 days.
Currently, I do not believe I experience any side effects.
Sympoms naltrexone helped me with#
Better temporal awareness#
When I experience a sufficient amount of stress, my awareness of time becomes very restricted. This makes it difficult for me to ground in the present time or to have an understanding of events both in the past and future. I lack temporal awareness, and am thus unable to understand where I am in life so my awareness of my present life becomes blurry—my life becomes timeless.
While I still have times of restricted awareness on naltrexone when I’m particularly stressed, it seems much less severe, with episodes of temporal confusion lasting much shorter (days on naltrexone vs weeks to months before starting). I am now moreso able to understand where I am in my life, and because of that it makes it easier to make decisions that allow me to advance in life. Naltrexone has enabled me to have a better grasp on the present with context about my past and future.
Improved facial recognition#
Before starting naltrexone, I often struggled with recognizing familiar faces. For example, on several occasions I would wake up next to my partner in the middle of the night and fail to recognize him, leading to panic and confusion. I would leave the bed to change into less revealing clothes before returning, only to slowly realize that this “stranger” was, in fact, my life partner. Similar situations occurred with my dad, where I would recognize him as a male figure in my life but confuse him for my brother or partner, occasionally starting conversations based on that misunderstanding.
Additionally, throughout my life, I have experienced numerous embarrassing moments where I would encounter friends or acquaintances in unfamiliar environments and completely fail to recognize them while they clearly recognized me. I have not had any obvious episodes of facial recognition issues since starting naltrexone, but when I briefly stopped taking naltrexone to assess its effects, I experienced a few instances of not recognizing people. When I started naltrexone again, these episodes stopped, providing me with sufficient evidence to believe that naltrexone has positively impacted my ability to recognize people. This improvement may relate to findings suggesting that opioid-mediated dysfunction in the amygdala contributes to recognition difficulties, which naltrexone could theoretically help mitigate (page 94-95).
More control over switches and deep thinking#
Perhaps because I am polyfragmented, I tend to switch very frequently. At my worst, I was consistently switching over 100 times a day, making life very disorienting. Sometimes this would involve rapid switching, which for me means switching several times a minute when there’s an acute stressor, but I also would just switch a lot regularly—oftentimes, I’d only be able to spend 10-20 minutes in a compartment at a time before switching, so I’d be disjointedly changing from task to task, not able to have a continuous memory of my day.
One notable way this manifested was during work. I am currently completing a PhD in mathematics. This requires thinking very deeply about abstract concepts, which means I need to maintain a steady focus and push through mental difficulties regularly. Before my dissociative symptoms started flaring, I was easily able to get into the correct mindset for this and was able to genuinely enjoy my work. However, when my dissociative symptoms started, it became very difficult to get into the correct mindset. Any time I’d encounter a mentally difficult problem, instead of pushing though it like I used to be able to, I would switch and end up in an entirely different mindset than the one I needed to be in—I’d all of a sudden find myself, say, in a VR game or staring at my fish tank when I should have been working.
Since starting naltrexone, I’m able to push through difficult problems much more easily—when I encounter a mental challenge, I can vaguely feel the pull to leave my desk and do something else, but I’m now able to push through it and thus advance in work. This has been immensely beneficial for my work. Because of this, I’ve made more academic advancements in the 8 months I’ve been on naltrexone than the previous 3+ years before that combined. This lines up with the hypothesis that opioids encourage passive defense responses and inhibit active ones—it was very difficult to push through mathematical road blocks before starting naltrexone, whereas now it’s actually enjoyable.
Feeling more emotions#
On naltrexone, I have a noticeably larger dynamic range of emotions than before. Granted, most of the time I still don’t know what these emotions are2, but at least I am feeling something, which is better than the nothing that I felt before. Before naltrexone, I hardly ever cried, maybe a few times a year. On naltrexone, there are periods where I tear up multiple times a day (I think mostly out of love?), which can be a lot for me.
My ability to connect with emotions comes and goes, however. I still do have periods where I feel emotionally detached and numb. I think it depends a lot on what current stressors I have and what I am processing at the time.
More experiences worth noting#
Increased anxiety after starting naltrexone#
A few weeks after starting naltrexone, I experienced a ~3 week period of increased intense anxiety. I would frequently play out every worst-case scenario in my life, would regularly wake up in the night with a racing mind, and could hardly sit still out of antsiness and anxiety. This was abnormal for me, as I typically don’t feel much anxiety. Everything seemed emotionally overwhelming for a few weeks, but then things stabilized.
I think what happened was that naltrexone reduced my dissociative symptoms enough that I was unable to use dissociation as a suitable coping mechanism anymore. It took some time to learn new coping mechanisms, but once I did, things became better. At the same time, naltrexone allowed me to ground in the reality of my life, which allowed me to realize how much I had lost due to my dissociation, so that also increased my anxiety.
Effects of standard-dose naltrexone#
Although I am currently taking 4 mg 3x a day of naltrexone which works well for me, when I first started naltrexone, I was prescribed 50 mg to be taken 1x a day, which is the standard dose of naltrexone. I decided to taper on and started at 12.5 mg, and I only took this dose 2 times before deciding to stop due to severe side effects. However, I immediately noticed that this affected my dissociative symptoms.
I took this dose for the first time ~1 hour before my therapy appointment, and during that appointment I had a pretty strong dissociative episode. I experienced complete switching to a traumatized part with amnesia, which came with intense emotion. I discretely switched back and forth between my “adult self” and this traumatized part several times in the session, and was unable to blend between the two compartments like I typically was able to. I only have a vague memory of what happened in the dissociative episode, but I journaled that I essentially was making connections through my past, present, and future, realizing how a seed of trauma from my early childhood affected me throughout my life. It seemed to break down barriers between parts, but I was unable to retain the insight I gained from the experience. I haven’t taken this dosage of naltrexone since then.
What naltrexone has not helped with#
I still do have dissociative symptoms, so naltrexone did not eliminate them entirely. Most notably, I do experience spaciness/detachment frequently, possibly at a similar rate prior to taking naltrexone, but it’s honestly hard to tell. For the most part, it seems like my dissociative experiences have been toned down, but not entirely eliminated. On naltrexone, it doesn’t feel like my internal experience has radically changed, which is good. The effects are very subtle and are moreso noticeable by looking at long-term trends.
Data analysis#
Apologies in advance to my non-data-minded readers, but I have a lot of data and nobody to share it with, so while you’re a captive audience, I’ll place it here. Also, I think the results I was able to compile show a compelling argument for how effective naltrexone has been for treating my dissociative symptoms.
I collect a lot of data about myself which has allowed me to gain insight about how I operate as well as orient myself in time. For the sake of this post, we can use this data to gain insight about my experience with naltrexone in two ways: determining the amount I have been able to work before vs after taking naltrexone, and displaying the time of day when I’ve been dosing naltrexone. I use TimeTagger to log hours worked, Binders to log my medication usage, and Python to process the data.
Hours worked before and after naltrexone#
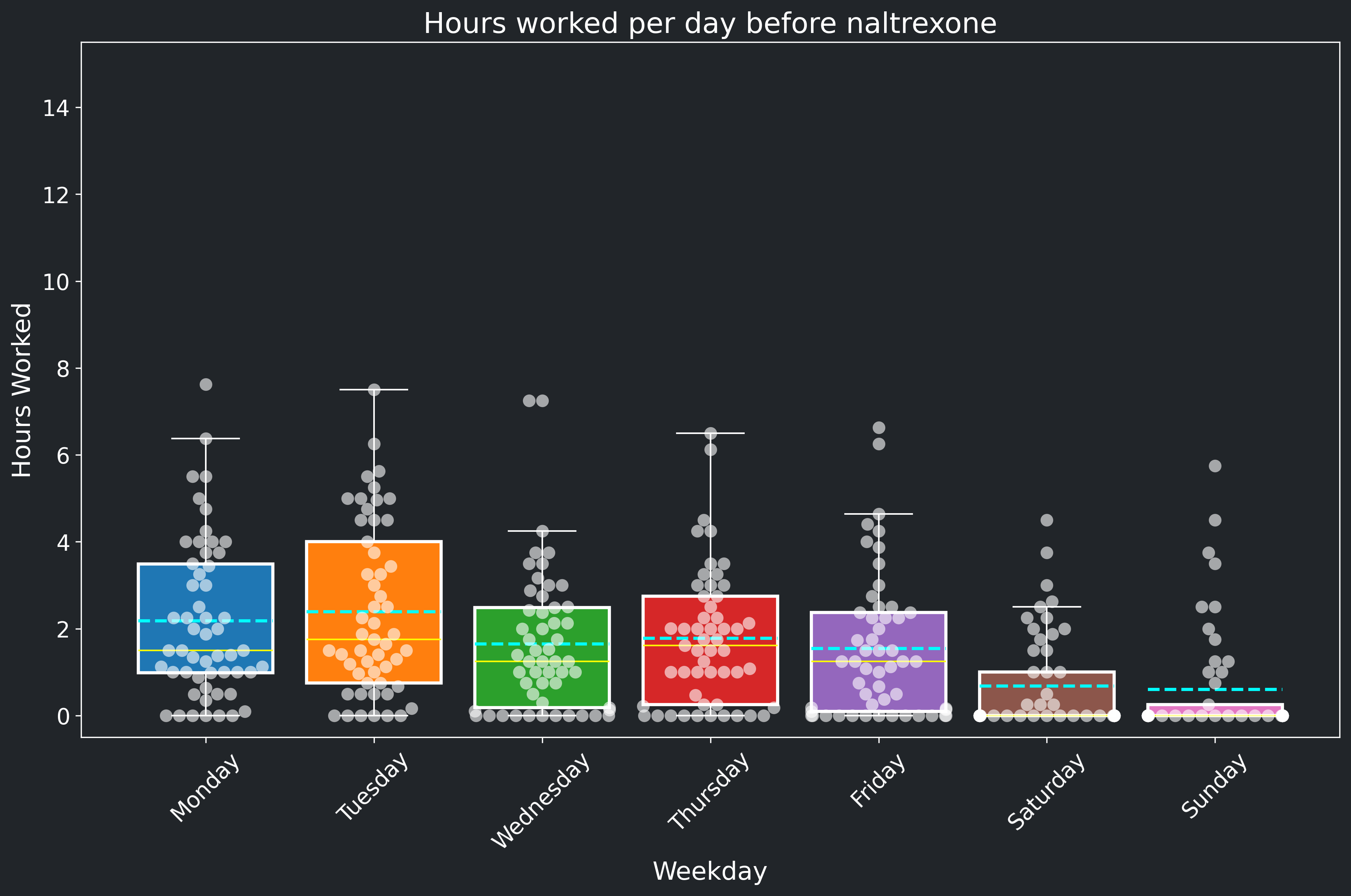
Naltrexone greatly improved my ability to get active work done, as I described in a previous section. This is plainly visible in two plots: How many working hours I logged before starting naltrexone (Figure 1), and my working hours since being on naltrexone (Figure 2). It’s clear from these plots that I was able to work much more while on naltrexone, but also the quality of that work was much better.
Before naltrexone, I was generally working a little bit every day (with many days that I didn’t work at all), but this wasn’t productive work. I tried working weekends as well because I felt that I was so far behind that I needed to in order to catch up, but it didn’t really help because I wasn’t actually making much progress even when I was logging work hours.
After naltrexone, I had a more consistent schedule—I was able to get work done when I wanted to, so I mostly concentrated my work on weekdays and took weekends off. This work was much more productive, too. I was able to reach the mental state required of me to advance in my research, which was very difficult to get to for any period of time prior to taking naltrexone.
Please be warned: like all data sets, there is bias in this data. First of all, there’s more time in the period before starting naltrexone than in the period since being on naltrexone, so I have more data and thus a better understanding of what my work history was before starting naltrexone than since being on naltrexone. Also, in the time period in Figure 2 (on naltrexone), there was a period where I briefly stopped naltrexone (in order to confirm what naltrexone was actually doing for me, plus taking it 3x a day is difficult). More importantly, during this period I had a 12 week summer internship, which means my work routine was different then than my typical graduate student schedule3. However, I don’t think these biases should detract from the clear benefit that naltrexone provided for my work life. For comparison sake, I recreate figure 2 excluding the time period of my summer internship here. For further clarity, the table in Figure 3 shows the median and mean hours worked for weekdays and weekends before naltrexone, after naltrexone, and after naltrexone excluding the time period of my summer internship.
| Number of hours worked | Median weekdays | Mean weekdays | Median weekends | Mean weekends |
|---|---|---|---|---|
| Before naltrexone | 1.50 | 1.91 | 0 | 0.64 |
| After naltrexone | 3.79 | 5.00 | 0 | 0.62 |
| After naltrexone, excluding internship | 3.01 | 3.27 | 0 | 0.39 |
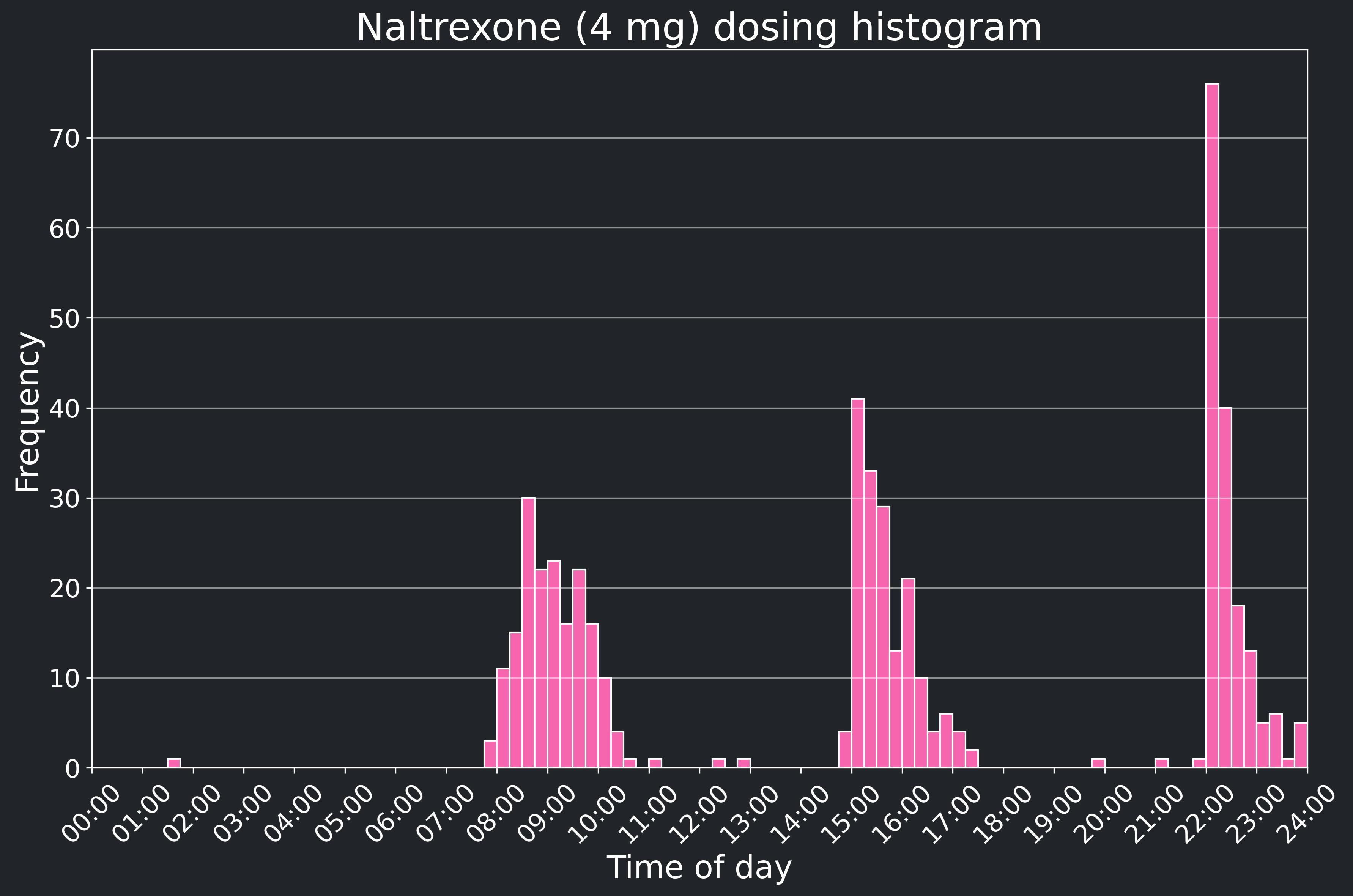
Time of day when I dose naltrexone#
So this is a less useful graph than the previous section, but I have the data, so I may as well display it? Anyways, I aim to take 4 mg naltrexone 3x a day. To remind myself, I set an alarm on my watch to go off at 8 AM, 3 PM, and 10 PM. Figure 4 shows the logged times of the day that I take naltrexone. As you can see, I’m pretty lax about precise timing, especially in the mornings, but it still seems effective to me.
Conclusions#
I believe naltrexone reduced my dissociative symptoms enough to allow me to gain alternative, less maladaptive coping mechanisms. This has allowed me to push through mentally difficult problems in work and advance in life. I can definitively say that I wouldn’t have made as much improvement in my life as I have over the past ~8 months if I hadn’t taken naltrexone. However, naltrexone isn’t a panacea—I still do have dissociative symptoms. But it has helped a lot, and the difference in my mental state before and after starting naltrexone is striking. I now am able to maintain a stronger mental focus, am feeling more emotions, and am more aware of and engaged in life. I strongly believe that, in combination with therapy, understanding how I operate, and time, naltrexone has played a crucial role in my healing journey so far.
-
Specifically clonidine, quetiapine, aripiprazole, and bupropion. I also have access to alprazolam for acute stressors. ↩︎
-
I’m still learning what these emotions are! It’s a lot of work, I’m confused about what I’m feeling much of the time. But I wasn’t able to access these emotions at all off of naltrexone—naltrexone is allowing me to feel them in the first place. Now my work is to try to understand what they are. ↩︎
-
When I log hours in grad school, I am only logging when I am actively working—when I take breaks, I stop the timer. During my internship, however, I started the timer when I entered the office and stopped it when I exited the office. This means there’s a difference in how I logged hours as well as my routine. However, during my internship I had to be “always on”, whereas as a grad student I work on my on schedule from home. Because of this, I genuinely did work more hours during my internship because that’s what was required of me, but those hours worked were much less mentally challenging (but much more socially challenging!) than hours worked as a grad student. ↩︎
Contact me